Story by Vardit Kohn
Illustration by Anna Temczuk
Until recently, there was no advocacy or central voice for the participants in clinical trials involving psychedelics. Now, there is PsyPAN, a non-profit organisation set up to connect and empower psychedelic participants. Founders Ian Roullier and Leonie Schneider both participated in such trials. Ian took part in the psilocybin for depression trials at Imperial College (2015) and Compass Pathways (2019). Leonie took part in the second phase of the psilocybin for depression study at Imperial College (2019) and the DMT for depression trial at Small Pharma (2022). They were later invited to take part in Dr. Rosalind Watts’ one-year integration programme, where they met.
Towards the end of the programme, Leonie and Ian discovered they had a shared interest – both in advocating for the spread of psychedelic treatment for mental health as well as having the patients’ perspective duly represented. No organisation representing the patient’s viewpoints existed, while the number of participants in psychedelic trials is increasing by the day. And as the standards for these novel treatments are now being developed, both felt that the voice of the patient needed to be heard louder.
So, in 2021, Leonie and Ian founded the Psychedelic Participant Advocacy Network: PsyPAN. It’s a non-profit organisation set up to connect and empower all psychedelic participants. PsyPAN aims to give a collective voice to all participants and help improve participant safety and wellbeing, by working on developing best practices across all levels of the global psychedelic sector – clinical and non-clinical alike.
As the psychedelic sector is expanding at a breathtaking pace, companies, clinicians and modern-day curanderos alike have a lot to learn from the persons seeking their help. We talked to Leonie and Ian for this interview.
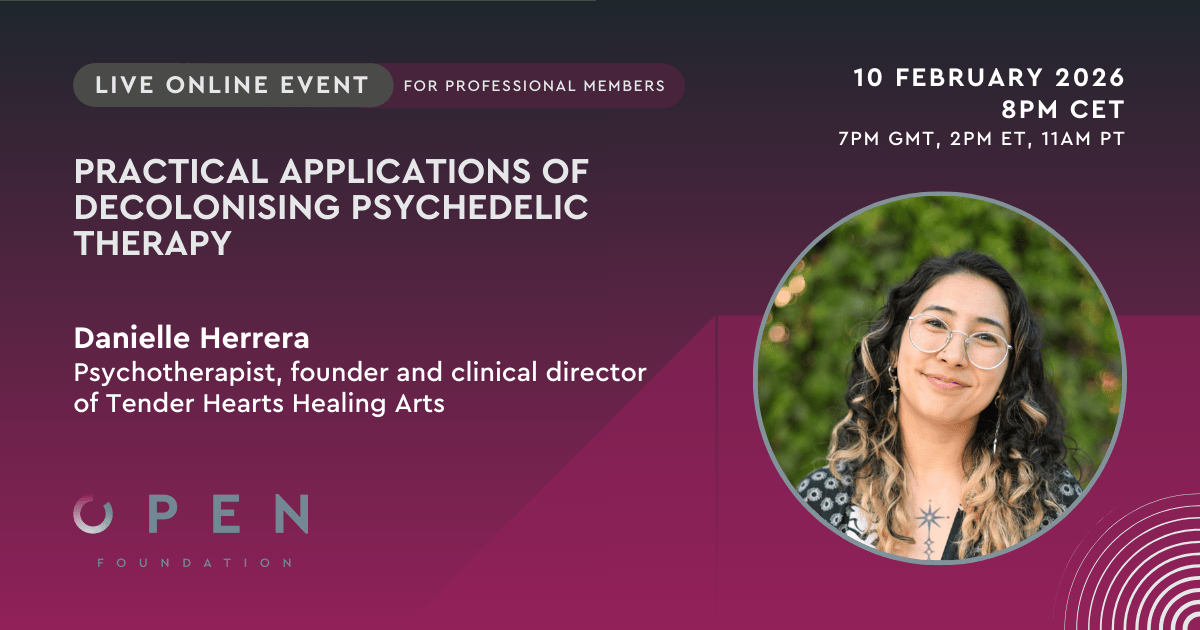
Leonie and Ian will also be speaking at ICPR 2022, the psychedelic conference organised by the OPEN Foundation, which has been promoting psychedelic research and therapy since 2007.
What motivated you to set up PsyPAN?
Ian: We both participated in clinical trials designed to test the effects of psilocybin and DMT on depression. Our wildly varied, but generally positive personal experiences triggered a wish to bring these treatments to more people and at the same time ensure the treatments are delivered safely and responsibly.
Leonie: We want to ensure the ‘participant’s voice’ is taken into account when clinical trials are designed, so that the trials can be tailored to meet the wide range of experiences. Despite some unifying themes across the psychedelic experience,, it is such a personal process, and deep trauma and psychological issues can present in so many different ways. We want to provide a feedback loop: taking what participants say, giving that to industry, and having industry respond to what participants require in this process. So that we can ensure these treatments are tailored and take nuances and details into account.
Ian: Next to the ‘participants’ voice’ we keenly engage in advocacy work, destigmatizing the image of psychedelics, dispelling misunderstandings and fear. We are keen to ensure that more people can benefit from these treatments in a safe and appropriate way.
ㅤ
ㅤ
Is psychedelic therapy especially prone to safety risks?
Ian: Yes, psychedelic therapy is more risky than, for example, giving someone an SSRI. Psychedelic substances lay you bare and much more vulnerable, you can’t just get up and go back to work as if nothing happened. It is also their strength; but therein also lies the potential for healing.
Leonie: Safety is therefore key, so developing psychedelic safeguarding guidelines is where we can help organisations.
Where do you see your contribution to the rapidly developing market of psychedelic therapy?
Ian: We work with organisations to ensure that they have the finer details in place, and we hope to develop a model of best practice that organisations could follow.
Leonie: Sometimes there are issues organisations simply haven’t thought of because those involved haven’t suffered from the issues that people with a clinical diagnosis have gone through, nor have they taken part in clinical trials, so our feedback is valuable. We aim to help ensure that trials or treatments are delivered safely and appropriately, because the more corners cut, the less effective the treatment will be.
What have you learned so far in the process that you were not expecting?
Ian: We found out that simply connecting people who have been through similar experiences is in itself of vital importance.
Leonie: Yeah. There is no community, or a place where you can go, to land after your experience. So it can be incredibly isolating. If you’ve been through a profound experience but can’t speak to anyone about it, you may still feel as isolated as you did pre-treatment, only in a different way. The circle of family and friends you go back to can’t necessarily understand what you have been through. We learned that there is a lot of value in simply creating a peer community for support.
ㅤ
ㅤ
If there was one thing you as participants in clinical trials would like to draw attention to, what would it be?
Ian : Open-label trials, in other words making sure that all participants who go through the process have access to a treatment dose. Contributing to science is wonderful, but if you’re so desperate as to be willing to participate in a clinical trial of a new substance, you really are in need of relief. To go through the process and only have a placebo is quite heartbreaking and potentially re-traumatising. To have access to the full treatment dose could therefore be life-saving for some.
Leonie: Integration. Both of us participated in Rosalind Watts’ “Connectedness” program at Synthesis Institute which was the precursor to Dr Watts’ ACER Integration Programme, which was hugely beneficial. It connected us in monthly group meetings and group work (two groups of 10 participants each) for one full year. The psychedelics are catalysts, they likely allow more progress to be made during the integration. But this kind of deep, long-term integration and connection work has been hugely beneficial.
Tell me more about Integration
Leonie: Having a space in which to integrate these experiences brought about by psychedelics is incredibly important, whether one-on-one or in a group, especially if the person has had long-term mental health issues. There is a need for longer-term and deeper level integration, not just a courtesy call of ‘how are you’. It’s about witnessing and supporting people every step of the journey.
As mentioned, we both participated in Rosalind Watts’ 1-year long “Connectedness” program. Due to Covid-19, the whole program was delivered online, which wasn’t the plan at all! And still it was so valuable. It kept many of us afloat, especially considering the pandemic. As long as there is a safe container, an online program can genuinely work.
The sweet spot could be to have online content enhanced with in-person meetings, hopefully in smaller, local groups (as treatments become more common) and outdoors, which allows for engagement with Nature.
What part did the connection with Nature play in your healing process?
Leonie: Reconnecting with Nature and with every living thing is very powerful. For example, watching the same tree go through its year-long cycle, especially during the dark, deathly-looking winter months, realising this period is part of a longer cycle, realizing there is still a lot happening under the surface even if above ground the tree looks barren – this was all very meaningful.
Most of mental illness is exacerbated by trying to avoid feelings as opposed to accepting them. When you learn to see low moods as “this is my Wintering, and Spring will come”, it creates a meaningful marker, a reference point.
What should organisations emphasise as the most important factors for a patient to consider before deciding to join a clinical psychedelic study?
Leonie: Organisations running clinical trials must make potential participants aware that the ‘trip day’ is just a catalyst. You’re in the process for the long run and there will be plenty of long-term, steady work that only starts after the day at the clinic. The importance of long-term integration and connection after the ‘trip day’ cannot and should not be underestimated.
Ian: Expectations should also be carefully managed regarding the chances of getting into the trial. Many people aren’t accepted. Furthermore, organisations would do well to question the kind of support networks potential candidates have in place, because a lot of support is needed right from the recruitment and screening stages. What further support is available during and after the treatment? Is there a community and family in place that can hold your experience, so you do not end up in crushing isolation, which might negate any benefit you could get from the treatment?
Organisations engaging in double-blind trials should also make it very clear that participants have a 50-50 chance of getting a placebo, which may result in disappointment. In the case of depression, you need to come off the anti-depressant medication, which makes you more vulnerable. You hope for an improvement but may end up with a placebo, with all the disappointment and anxiety this may cause. You may potentially end up in a worse position than you were before entering the trial.
To what extent if any does treatment with different psychedelic substances require different guidelines?
Leonie: It is certainly important to bear in mind what medicine you’re working with and then tailor the guidelines appropriately since the experiences vary in intensity, the type of in-session interaction and the kind of post-treatment support required depending on the medicine used. Furthermore, the theme of the session matters, too. As an example, if sexual issues are likely to arise, two therapists present and a recording of the sessions may provide more accountability.
How could the current positive hype around psychedelics impact patients and therapists?
Ian: There’s a risk in the current media hype for psychedelic therapy to be seen as a ‘one dose and you’re fixed forever’ treatment. It sets expectations too high, and, in the absence of legal treatments, people may opt to try the psychedelics themselves without appropriate support.
Psychedelics are catalysts, not cures. In reality, when it comes to mental health a lot of the healing work happens afterwards. It’s a long process that involves a lot of integration and support going forward. The focus should be more on the psychotherapy, not completely on the psychedelic aspect of the process. If this point isn’t made clear, the risk is that the treatments will be seen as ineffective, which would be a shame as there is huge potential in psychedelics.

How do participants’ opinions get heard through you?
Leonie: Participants who have been through the clinical trial setting are the ones most interested in our work, We raise awareness within organisations who run such trials and invite participants informally to join our efforts. Going forward, we want references to PsyPAN to be built into the treatment protocol so that participants can be seamly signposted to us and welcomes to participate if they choose to.
Speaking at ICPR and other events where participants are present is another way of creating awareness of our work. We also help organisations put together a working or focus group, so participants can share their experiences and have a say in the way trial protocols are designed.
Ian: As far as we know, there’s nobody doing exactly what we’re doing. If there are other such groups or networks, we will be delighted to connect with them and support each other. We’re all doing it for the greater good of people who are struggling with mental health conditions.
How do you view depression, as you were both treated for it.
Leonie: Depression is a disease of disconnection. In society we are disconnected in so many ways. Depression alerts us to a deep need to slow down, take deep rest and to reconnect: to Nature, to ourselves, to our feelings – all of them, including the painful ones.
Ian: We live in a world where we’re atomized and isolated, and the pandemic only exacerbated that. We are raised to dismiss a large part of our emotional range as human beings. We try to deny the more challenging parts of ourselves and our histories.
Leonie: Antidepressants are a powerful intervention when you are in an acute, overwhelming crisis. But they should be seen as a short-term, symptom management intervention. They should not be viewed as something that is taken indefinitely, as if depression was a terminal disease that you had to learn to live with, as they don’t just numb you to the negative emotions; they limit and numb you in many other ways, too. If you don’t deal with the underlying causes of your depression, the issues come up in a different way at a different time.
Ian: Psychedelics work in the completely opposite way: they enable you to connect with your full range of emotions and learn to be comfortable with your fuller self. Psychedelics help you dig down to the roots of your depression and work out new ways to deal with difficult feelings within a natural container that is larger than just yourself.
You mentioned several spiritual themes: connection to Nature, connection to something that is larger than us, the Cycle of Life. How does that sit with the current clinical, medical training?
Leonie: No participant or clinician starts the trial thinking clinically-diagnosed patients need more trees in their life… We must be careful not to be too reductionist – depression is not solely a function of neurochemistry. There needs to be some space for mystery, too.
Ian: Psychedelics can engender deeply profound spiritual experiences, which can manifest in different ways; we must not be prescriptive as to the nature of the spiritual experience to be expected. Yet organisations who run the studies must be aware that these experiences do happen.
Leonie: The concept of connectedness is a good place to start. Everyone can understand how being better connected to ourselves, each other and Nature is beneficial to all. It is definitely a point to bring to the discussion, otherwise we will be selling the psychedelic treatment short.