Abstract
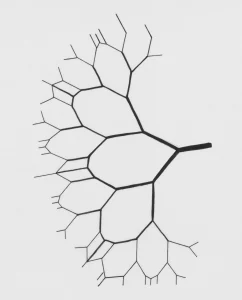
Capitalizing on recent advances in resting state functional connectivity magnetic resonance imaging (rs-fcMRI) and the distinctive paradigm of rapid mood normalization following ketamine treatment, the current study investigated intrinsic brain networks in major depressive disorder (MDD) during a depressive episode and following treatment with ketamine. Medication-free patients with MDD and healthy control subjects (HC) completed baseline rs-fcMRI. MDD patients received a single infusion of ketamine and underwent repeated rs-fcMRI at 24 h post-treatment. Global brain connectivity with global signal regression (GBCr) values were computed as the average of correlations of each voxel with all other gray matter voxels in the brain. MDD group showed reduced GBCr in the prefrontal cortex (PFC), but increased GBCr in the posterior cingulate, precuneus, lingual gyrus, and cerebellum. Ketamine significantly increased GBCr in the PFC and reduced GBCr in the cerebellum. At baseline, 2174 voxels of altered GBCr were identified, but only 310 voxels significantly differed relative to controls following treatment (corrected α<0.05). Responders to ketamine showed increased GBCr in the lateral PFC, caudate, and insula. Followup seed-based analyses illustrated a pattern of dysconnectivity between the PFC/subcortex and the rest of the brain in MDD, which appeared to normalize post-ketamine. The extent of the functional dysconnectivity identified in MDD and the swift and robust normalization following treatment, suggest that GBCr may serve as a treatment response biomarker for the development of rapid acting antidepressants. The data also identified unique prefrontal and striatal circuitry as putative marker of successful treatment and target for antidepressants development.
Abdallah, C. G., Averill, L. A., Collins, K. A., Geha, P., Schwartz, J., Averill, C., … & Iosifescu, D. V. (2016). Ketamine Treatment and Global Brain Connectivity in Major Depression. Neuropsychopharmacology: official publication of the American College of Neuropsychopharmacology. 10.1038/npp.2016.186