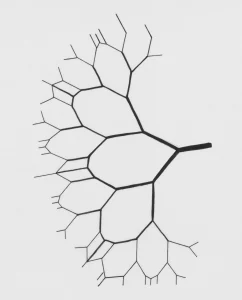
Serotonin is a key neuromodulator known to be involved in brain development, perception, cognition, and mood. However, unlike as with dopamine for example, a compelling unified theory of brain serotonin function has not yet been established. This is likely due to the exceptional complexity of the serotonin system, with its 14+ receptors, over twice the number identified for any of the other major neuromodulator systems.
Serotonin has been implicated in several major psychiatric disorders, and most obviously in depression. Chronic medication with selective serotonin reuptake inhibitors (SSRIs) remains the dominant treatment for unipolar depression, and SSRI prescription rates have been increasing year‐on‐year at record levels. Such widespread SSRI use has not noticeably impacted on depression prevalence, however, and questions continue to be asked about the safety, efficacy and general philosophy of chronic pharmacotherapy.
Historically, psychiatry has been a divided house, with the psychodynamic model dominating the first half of the 20th century, and the biomedical model ever since. It is natural for early perspectives within nascent disciplines to overshoot in confidence before maturing and moderating over time. Such has been the case with psychodynamic psychology for example, and there are reasons to suspect that something similar may be happening in relation to the pharmacological model.
This subtle shift in perspective is especially evident in contemporary serotonin and depression research. Until recently, it was not unusual to hear patients, doctors and even psychiatrists speak with presumed authority about how deficient serotonin functioning is causal of depression, offering solace in the view that “serotonin is to blame”. As with genetic determinism, one should be mindful of the emotional function of such explanations – especially in psychiatry, the most personal of medical disciplines.
So what is the relationship between serotonin and depression? A fair (but unsatisfactory) answer to this question is that “it is complex”. Not wishing to sit on the fence, however, a more constructive statement is that there is increasing evidence that serotonergic processes play a critical role in mediating an individual’s sensitivity to context. For example, within the last decade, seminal work has been done to demonstrate how genetic variation within and pharmacological manipulations of the serotonergic system interact significantly with environmental factors to determine outcomes in mental health. The natural implication is that the pure pharmacological model can explain only part of the mental health picture.
What, then, is the alternative? By implication, we should be looking for a hybrid model, a middle‐way, that combines the precision, potency and cost‐effectiveness of biomedicine with the depth of insight and roundedness of psychology. There is already evidence that SSRIs, in combination with evidence‐based psychotherapies, offer (marginally) superior efficacy over either treatment alone – but should our search stop here?
In 1975, the Czech psychiatrist S. Grof compared the potential impact of psychedelic drugs on psychiatry to that of the microscope on biology and, while this analogy may strike some as laughable, let us reflect for a moment that human research with psychedelics has been effectively moribund since the restrictive drug policy reforms of the 1960s‐70s, and has only recently been revived.
Classic serotonergic psychedelics – such as LSD, psilocybin and dimethyltryptamine – all possess agonist properties at the 5‐HT2A receptor subtype, and 5‐HT2A receptor agonism is known to be the pharmacological trigger of the “psychedelic experience”. Crucially, there is also a wealth of evidence to implicate 5‐HT2A receptor signaling in processes of plasticity, such as neurogenesis, neurodevelopment, learning, extinction learning, cognitive flexibility and enhanced environmental sensitivity.
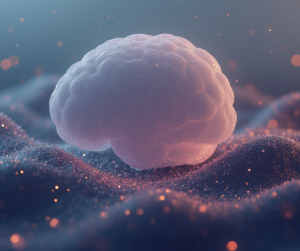
Added to this, the subjective quality of a psychedelic experience is highly susceptible to contextual influence, for example from the environment in which it occurs as well as from the expectations of the “tripper” and those around him or her. Moreover, the quality of an acute psychedelic experience appears to be a highly reliable predictor of subsequent long‐term mental health outcomes. Another predictor of long‐term psychological outcomes is the degree of increase in the complexity or “entropy” of brain activity recorded during the psychedelic experience, and this brain effect is hypothesized to be relatively unique to psychedelics, and key to an understanding of their exceptional phenomenology and therapeutic potential.
Within the last 12 years, a growing body of evidence, albeit from mostly small scale pilot studies, has suggested that psychedelics, combined with contextual manipulation (such as music listening and psychological support), can offer a safe and effective treatment for a range of different psychiatric disorders. Where successful, the treatment effect appears to be rapid and enduring. Moreover, promising outcomes have not just been seen in depression, but in addiction and other disorders as well. That just one or two treatment sessions can yield therapeutic effects lasting for several months is unprecedented in modern psychiatry. Of course, incredible claims require credible evidence but, with large randomized controlled trials beginning with psilocybin for depression, the required roads are being laid.
A simple and plausible model of therapeutic mechanisms of psychedelic treatments would greatly complement this ongoing clinical work. The thesis is put forward here that serotonin differentially encodes behavioral and physiological responses to uncertainty. More specifically, it is proposed that the limbic‐rich inhibitory postsynaptic 5‐HT1A receptor subtype provides basal control during normal conditions, via moderating emotion and anxiety, and promoting a generalized patience. On the other hand, the cortically‐rich 5‐HT2A receptor subtype is hypothesized to engage more during conditions of crisis, when the above‐mentioned default mechanism becomes suboptimal, e.g. when an individual’s internal and/or external milieu becomes so changeable and/or inconsistent with his/her prior beliefs and behaviors that significant revisions become mandated.
Viewed through a Bayesian lens, it is proposed that the principal functional effect of 5‐HT2A receptor stimulation is to relax prior assumptions or beliefs, held at multiple levels of the brain’s functional hierarchy: perceptually, emotionally, cognitively and philosophically (e.g., in terms of biases). In so doing, it opens a door to heightened sensitivity to context, an ideal pre‐condition for effective change.
Carhart‐Harris, R. L. (2018). Serotonin, psychedelics and psychiatry. World Psychiatry, 17(3), 358., 10.1002/wps.20555
Link to full text