A European consortium of 19 partners, which includes the OPEN Foundation, has been awarded over €6.5M by the European Union to study psilocybin to treat psychological distress in people with progressive incurable illnesses requiring palliative care. This is the first time the EU has funded a multi-site clinical study into psychedelic-assisted therapy.
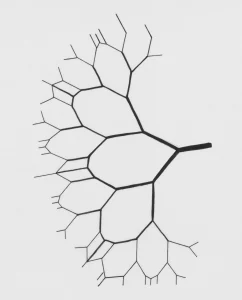
The randomised controlled trial (RCT) PsyPal, coordinated by the University Medical Centre Groningen in the Netherlands, and in collaboration with HumanKindLabs, marks the first-ever European grant to fund clinical research into psychedelic-assisted therapy. The trial will investigate whether psilocybin therapy can help ease psychological and existential distress in patients suffering from one of four different progressive diseases: the lung condition chronic obstructive pulmonary disorder (COPD), multiple sclerosis (MS), amyotrophic lateral sclerosis (ALS, also known as MND), and atypical Parkinson’s disease (APD).
Commencing in early 2024, the PsyPal study will launch with the aim of treating over one hundred patients across four distinct clinical sites where each focuses on a specific condition: COPD at the University Medical Centre Groningen (UMCG) in the Netherlands, APD at the Champalimaud Foundation in Portugal, MS at the National Institute of Mental Health in the Czech Republic, and ALS, jointly at the University of Copenhagen and the Bispebjerg Hospital in Denmark.
Participants will undergo two therapy sessions, receiving psilocybin (the active ingredient in psychedelic or ‘magic’ mushrooms) or a placebo. Previous pilot studies have shown substantial reduction in depressed mood and anxiety in people living with a terminal cancer diagnosis, with sometimes persistent benefits.
PsyPal marks the first clinical trial studying the safety and effects of psilocybin in non-oncology palliative care patients. Robert Schoevers, head of psychiatry at the UMCG and principal investigator of PsyPal notes: “We are eager to see if we can ease the suffering of these patients whilst also examining longer-term patient and family outcomes of this treatment, something that often gets overlooked but that is of enormous importance.”
European funding
This first-of-its-kind clinical trial is fully funded by Horizon Europe, the European Union’s key funding program for research and innovation. Horizon Europe aims to foster collaboration, bolster the impact of research and innovation, and address global challenges through the facilitation of EU policies.
Schoevers says, “We are absolutely thrilled that the EU is supporting this ambitious collaborative study. There is growing recognition that psychedelic treatments may help patients for whom alternatives are not effective, and I am very glad we are receiving support from this highly prestigious funding program. It really helps to strengthen the collaboration between researchers from different countries and disciplines, focusing on potentially transformative interventions for severe, currently treatment-resistant mental disorders.”
Joost Breeksema, executive director of the OPEN Foundation, enthusiastically says: ”This is a major milestone for many reasons: we are getting unequivocal financial support from the EU, we are further developing psychedelic-assisted treatment for novel indications (including neurodegenerative and lung diseases) and we are further establishing the Netherlands as a country on the forefront of psychedelic research and therapy in Europe. We are proud to be a partner in this consortium, and to join a wider group of therapists and researchers involved in using psychedelics to address people’s needs in the palliative phase of their illness.”
Psychological and existential distress
All four diseases are incurable and profoundly life-altering, leading to a loss of autonomy and severe psychological distress. Studies indicate that depression and anxiety symptoms affect 34% to 80% of individuals across these conditions, emphasising the pressing need for innovative interventions.
The impact of life-limiting or life-threatening illnesses on one’s physical, emotional, social, and spiritual well-being is profound. While some experience personal growth, others are confronted with a multitude of existential struggles, such as loss of hope and meaning, changes in family and societal roles, and feelings of burden. Consequently, depression, anxiety, demoralisation, and decreased quality of life are highly prevalent among these patients. Conventional interventions often fall short for these palliative care patients. This necessitates the need for innovative and effective treatments, such as psilocybin therapy.
Innovative therapeutic approach
Recent research in psychedelic science, particularly centred on psilocybin, has demonstrated promising therapeutic outcomes for individuals grappling with depression and spiritual distress due to incurable illnesses, such as cancer. Psychedelic-assisted psychotherapy, which integrates the use of psilocybin in a secure setting alongside professional psychological support, is introducing an innovative therapeutic approach that addresses not just symptoms of depression and anxiety but also promotes spiritual well-being and quality of life in palliative care patients.
PsyPal combines psychotherapy and pharmacotherapy to address these deep-seated human needs in these terminal conditions. Beyond immediate clinical outcomes, it targets sustained well-being for patients and their families post-psilocybin treatment. Using peer support and online tools, the project aims to enhance coping mechanisms and alleviate distress as people approach the end of their lives.
Collaborative and interdisciplinary consortium
This pioneering approach results in not just a clinical trial, but an interdisciplinary partnership consisting of 19 collaborating European organisations from 9 different countries. The consortium brings together a wide variety of specialists, including psychiatrists, palliative care physicians, psychologists, and experts in psilocybin therapy, alongside researchers focusing on spiritual care and representatives from religious institutions.
Breeksema: ”As OPEN, we’ll be jointly responsible to make sure that patients have continuous access to (peer) support, not just during the clinical trial phase, but also afterwards. This may be a difficult phase for people, and we think it is crucial to provide extensive support, enabling participants to process profound and sometimes difficult experiences.”
PsyPal Partners
The following organisations are part of the PsyPal consortium (listed alphabetically): 29k, A+ Science, Bispebjerg Hospital, Champalimaud Foundation, European Association for Palliative Care (EAPC), European Federation of Neurological Associations (EFNA), European Psychiatric Association (EPA), HumanKindLabs, IESE Business School, Lung Alliance Netherlands, Madopa, National Institute of Mental Health in the Czech Republic, Norrsken Mind, OPEN Foundation, University Medical Center Groningen (UMCG), University of Copenhagen, University of Groningen, University of Stockholm, Uppsala University.
In addition, the PsyPal consortium will be also actively engaging with PAREA (the Psychedelic Access and Research Europe Alliance).
The partners in the research consortium are committed to upholding the highest ethical standards in clinical and research practices, as laid out in the Horizon Europe regulation. Furthermore, the consortium will adhere to any requirements or recommendations from ethics committees and the regulatory authorities.

Disclaimer – PsyPal is funded by the European Union. Views and opinions expressed are however those of the author(s) only and do not necessarily reflect those of the European Union or the Health and Digital Executive Agency. Neither the European Union nor the granting authority can be held responsible for them.
Image credit: University Medical Centre Groningen (UMCG)