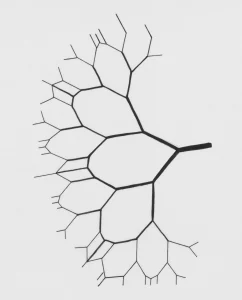
Picture this: you’re driving down a busy highway when suddenly an accident blocks the road. Emergency services rush in to clear the wreckage, but the real chaos starts afterwards as traffic jams and chain-reaction crashes ripple far beyond the initial point. This is a bit like what happens when a blood clot blocks an artery in the brain, leading to an ischemic stroke.
The initial interruption of blood flow is only part of the story; much of the damage comes later, as oxygen shortage (hypoxia), swelling, and inflammation spread through the system (ischemic cascade), and a disrupted blood-brain barrier (a sort of security fence around the brain) breaks down, leading to further swelling, increased neuroinflammation, and infiltration of immune cells into the brain, worsening a feedback loop that only amplifies itself. Undoubtedly, a scary picture.
Now, imagine if a compound best known for blasting the mind on cosmic journeys through hyperspace could also act like a traffic controller, calming the chaos, preventing those secondary accidents, and providing new roads for the highway to resume normal functioning. That’s what a team of researchers at Semmelweis University and the Institute of Biophysics, HUN-REN Biological Research Centre in Hungary, Europe, explored in a recent paper published in the journal Science, looking at the effects of N,N-dimethyltryptamine (DMT) on experimental models of stroke.
What the study did and found
In their study, researchers administered DMT after transiently blocking a brain artery in rats, inducing a controlled ischemic stroke, and observed something remarkable: the rats that received DMT had smaller areas of dead brain tissue (the ischemic penumbra), less swelling, and a stronger blood–brain barrier. In parallel, researchers tested cultured neurons and immune cells, observing that DMT significantly reduced the release of inflammatory molecules and prevented microglia—the brain’s resident “emergency responders”—from overreacting in destructive ways. The researchers also traced much of this effect to a molecular switch called the sigma-1 receptor, which has long been thought to have a crucial role in helping cells cope under stress. This observation provides a more complete mechanistic account of the effects that they observed in animal models.
Why this matters for stroke care
For decades, stroke has been one of medicine’s most frustrating frontiers. Even when blood flow is medically restored quickly, patients often suffer long-term damage from the secondary effects of the ischemic cascade. And even though ischemic events do activate a state of heightened brain plasticity, making the brain extremely responsive to training, the time window available after noticing and interrupting a stroke is often too short for subsequent motor and cognitive therapies to yield successful levels of recovery. In fact, there was a time when it was believed that inducing a second stroke could be a very successful strategy to reopen this critical period and provide a controlled new window for therapies to yield full recovery (of course, this was only experimentally observed in animal models). Given that therapeutic induction of a second stroke wouldn’t (shouldn’t!) be approved by an ethical committee, finding a compound that can step in and reduce the system’s fallout continues to be a long-sought holy grail for neuroscientists. Enter: “The Spirit Molecule”.
A rare, system-wide mechanism
In isolation, this study stands out for its holistic and mechanistic perspective. Instead of focusing only on brain tissue or isolated neurons, it shows how DMT’s action on the sigma-1 receptor stabilizes the brain’s blood vessels, supporting the integrity of the barrier that protects them, restores the function of astrocytes (non-neuronal support cells found in the central nervous system), and dampens the activity of the immune system all at once. That level of broad, system-wide effect for a drug is very rare, promising, and especially powerful when we contextualize these with previous findings. DMT had previously been observed to attenuate, via the sigma-1 receptor, the spreading depolarization and subsequent neuronal death that follow stroke. This spreading depolarization is characterized by a wave of massive neuronal and glial cell hyperactivity that propagates across the brain, followed by a suppression of electrical activity and an ion imbalance that leads to neuronal death and brain tissue degeneration. In vitro studies have also shown that DMT exerts potent protective effects against hypoxia in human cortical neurons and microglia, and that these effects require sigma-1 receptor activity. Finally, both in vitro and in vivo, DMT has been found to regulate adult neurogenesis, promoting neural stem cell proliferation and migration, generating new neurons, and improving spatial learning and memory. And it seemingly does so through, you guessed it, sigma-1 receptor activation.
From bench to bedside: what could come next
Pieces of fundamental research like these are foundational for medical breakthroughs to happen down the line, providing mechanistic and functional insights that can (and do) inspire and justify countless clinical trials. For example, Algernon Neuroscience, a private subsidiary of Algernon Pharmaceuticals, is developing DMT pamoate and nicotinate (novel salt forms of DMT) as potential treatments for ischemic and hemorrhagic stroke, which have already gone through Phase 1 and have a Phase 2 clinical trial planned for the last quarter of 2025. Additionally, given the cumulative evidence pointing to the sigma-1 receptor’s seemingly clear involvement, these discoveries could help scientists design other medicines inspired by DMT but optimized for clinical use.
Beyond sigma-1: critical periods and longer-acting psychedelics
DMT hits targets beyond the sigma-1 receptor, which overlap with other psychedelics. On that note, in their –dare I say, seminal– paper from 2023, Gül Dölen’s lab at Johns Hopkins University found that different classes of psychedelics converge in their capacity to reopen critical periods in the adult brain, and that the duration of this reopening is proportional to the length of the acute subjective effects reported in humans. While their work focused on the social reward learning critical period, combining all these findings could provide a solid scientific rationale for investigating whether longer-lasting psychedelic-based treatments, such as LSD, might produce a more prolonged window during which post-stroke physical and cognitive therapies could achieve full recovery rates.
Implications for the psychedelic science movement
Studies like the present one provide more reasons to believe that these compounds are not just about mystical journeys or even therapy sessions for depression and PTSD. They may also hold potential to treat devastating neurological conditions like stroke, which, at least theoretically, should not require any subjective experience as an essential component of a healing process. That alone expands the conversation and the credibility of psychedelic science, and contributes to the reframing of DMT itself, emerging from an Amazonian gateway to visionary realms now reimagined as a medicine that might help improve lives in neurology units. Finally, they suggest that its role in biology might be more fundamental and extend inwards beyond exogenous psychedelic experiences (though, as truly tempting as it is, I’ll reluctantly save the discussion of endogenous DMT presence and function for another time). Quite fittingly, this dual mystical-medical identity captures the spirit of the psychedelic renaissance.
Of course, it’s still early days. All the studies discussed are preclinical, conducted in vitro or on animals rather than humans. Yet the fact that such results are even on the table is enough to inspire cautious optimism and excitement, as stroke remains one of the leading causes of death and disability worldwide, and the intersection of psychedelics with that reality is a story worth watching closely.
References
- N,N-dimethyltryptamine mitigates experimental stroke by stabilizing the blood-brain barrier and reducing neuroinflammation: https://www.science.org/doi/10.1126/sciadv.adx5958
- Paradoxical motor recovery from a first stroke after induction of a second stroke: re-opening a post-ischemic sensitive period: https://pmc.ncbi.nlm.nih.gov/articles/PMC4930432/
- N,N-Dimethyltryptamine attenuates spreading depolarization and restrains neurodegeneration by sigma-1 receptor activation in the ischemic rat brain: https://www.sciencedirect.com/science/article/pii/S0028390821001660?via%3Dihub
- The Endogenous Hallucinogen and Trace Amine N,N-Dimethyltryptamine (DMT) Displays Potent Protective Effects against Hypoxia via Sigma-1 Receptor Activation in Human Primary iPSC-Derived Cortical Neurons and Microglia-Like Immune Cells: https://pmc.ncbi.nlm.nih.gov/articles/PMC5021697/
- DN,N-dimethyltryptamine compound found in the hallucinogenic tea ayahuasca, regulates adult neurogenesis in vitro and in vivo: https://www.nature.com/articles/s41398-020-01011-0
- Algernon Neuroscience “DMT Program for Stroke”: https://algernonneuroscience.com/dmt-program-for-stroke/
- Psychedelics reopen the social reward learning critical period: https://www.nature.com/articles/s41586-023-06204-3
AUTHOR

MSc in Fundamental Neuroscience, PhD candidate in Psychedelic Neuropharmacology
Sergio is a PhD student with a passion for understanding how psychedelics reshape the brain.
His academic journey began with a degree in Biotechnology from the Universidad Politécnica de Madrid. He then completed a traineeship in regenerative neuroscience at the GlowLab at the University of Zagreb. Following this, he pursued a Research Master’s in Cognitive and Clinical Neuroscience at Maastricht University in the Netherlands, where his fascination with the neurobiology of psychedelics developed.
Sergio was awarded the atai Fellowship for the Neuroscience of Psychedelics, which allowed him to join the Center for the Neuroscience of Psychedelics (CNP) at Massachusetts General Hospital, Harvard Medical School.
As a PhD student at the CNP, he specializes in fundamental research to investigate how natural and synthetic psychedelics, along with other neuroplasticity modulators, can drive structural and functional changes in the brain.
Beyond the lab, Sergio actively contributes to the psychedelic science ecosystem as a Scientific Dissemination volunteer at the OPEN Foundation.