In the 1950’s, research on the psychoactive properties of lysergic acid diethylamide (LSD) led scientists to the serotonin hypothesis of schizophrenia, a theory still used to explain the neurochemical roots of schizophrenia. Today, Höflich et al. (2015) have used ketamine to explore the role of neurotransmitter glutamate in this mental disorder [3].
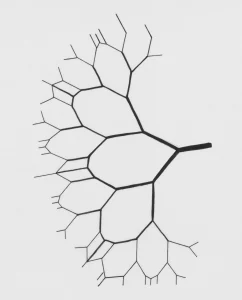
Since neuroimaging studies indicated dysfunctional glutamate pathways in schizophrenia, glutamate is thought to play a key role in its aetiology. These abnormalities are specifically apparent in the thalamus, a brain region regarded as the information integration system of the brain. By measuring brain activity in healthy volunteers after ketamine administration, Höflich et al. (2015) explored ketamine as a model for schizophrenia to further investigate the link between glutamate and schizophrenia. Ketamine is a glutamate antagonist, which means that it prevents neurotransmission by blocking the activity of glutamate on N-methyl-D-aspartate (NMDA) receptors. The effects of ketamine resemble some of the positive, negative, and cognitive symptoms of schizophrenia.
In the study of Höflich et al. (2015), thirty healthy volunteers completed a double-blind, placebo-controlled, randomized, crossover study in which each volunteer was scanned using fMRI on two separate days. Brain network activation under ketamine was compared to placebo. The brain images revealed higher functional connectivity in the thalamus hub network in the ketamine condition compared to placebo. Furthermore, ketamine induced higher connectivity between thalamic regions and somatosensory and temporal cortices. Connectivity between the thalamus and prefrontal, motor, posterior parietal, and occipital cortices did not differ significantly.
The authors conclude that ketamine temporarily triggers alterations in functional connectivity in healthy volunteers that resemble structural brain connectivity patterns in schizophrenic patients. They infer that the ketamine-induced state might function as a model of schizophrenia, especially relative to characteristic sensory filtering problems. However, their results did not reveal a decrease of prefrontal-thalamic connectivity typical for schizophrenic patients [4] suggesting that other neurotransmitters also account for the manifestation of schizophrenia. Using ketamine and other drug models [5] to investigate the relationship between neurotransmitter systems and the symptomatology of schizophrenia could yield valuable information about the neural underpinnings of this mental disorder.
[1] Gaddum, J. H., Hebb, C. O., Silver, A., & Swan, A. A. B. (1953). 5-Hydroxytryptamine. Pharmacological action and destruction in perfused lungs. Quart. J. Exper. Physiol., 38, 255.
[2] Woolley, D. W., & Shaw, E. (1954). a Biochemical and Pharmacological Suggestion About Certain Mental Disorders. Proceedings of the National Academy of Sciences of the United States of America, 40(4), 228–231. doi:10.1073/pnas.40.4.228
[3] Höflich, A., Hahn, A., Küblböck, M., Kranz, G. S., Vanicek, T., Windischberger, C., …Lanzenberger, R. (2015). Ketamine-Induced Modulation of the Thalamo- Cortical Network in Healthy Volunteers As a Model for Schizophrenia. International Journal of Neuropsychopharmacology, 1–11. doi:10.1093/ijnp/pyv040 [Abstract]
[4] Leitman DI, Sehatpour P, Higgins BA, Foxe JJ, Silipo G, Javitt DC (2010) Sensory deficits and distributed hierarchical dysfunction in schizophrenia. Am J Psychiatry 167:818–827
[5] Steeds, H., Carhart-Harris, R. L., & Stone, J. M. (2014). Drug models of schizophrenia. Therapeutic Advances in Psychopharmacology, 5(1), 43–58. doi:10.1177/2045125314557797 [Abstract][/fusion_builder_column][/fusion_builder_row][/fusion_builder_container]