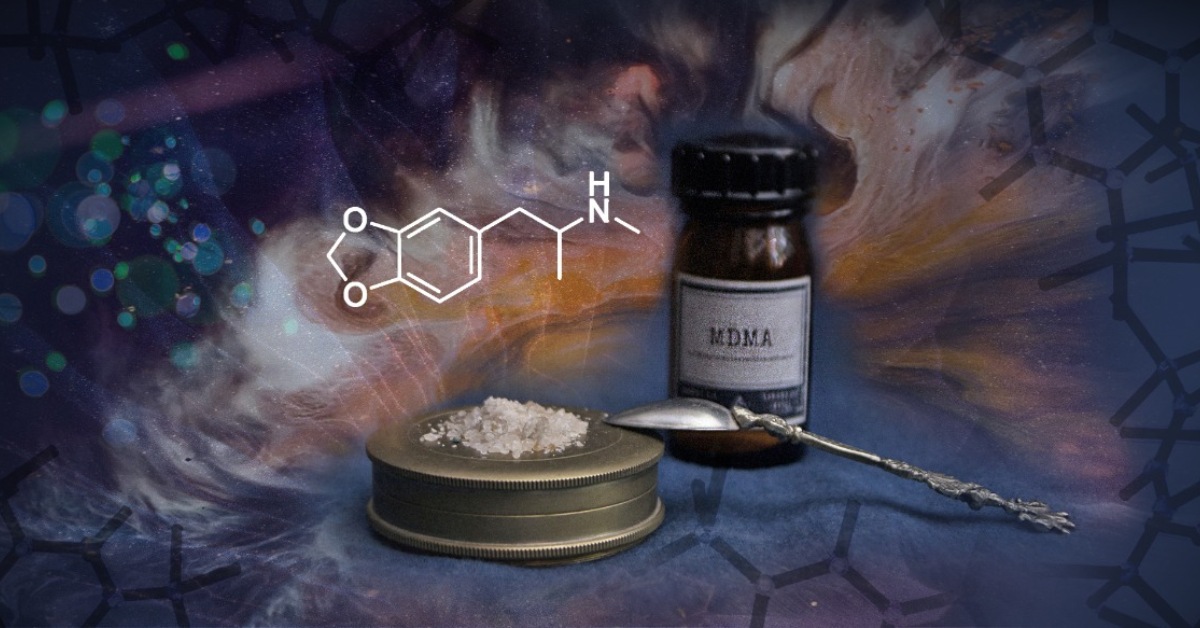
There has been a renaissance in the research of psychedelics, and much of it has been led by promising studies over the past two or three decades. Aside from the discussion of whether MDMA is a true ‘psychedelic’, it is clear that recent studies have created momentum to reconsider these substances as medication for severe mental health problems such as depression, anxiety or addiction.
MDMA’s application to trauma therapy has become one of the central priorities of psychedelic researchers. So what is the current state of knowledge and where do we stand in the regulatory process? According to MAPS-founder Rick Doblin, MDMA will be legal soon if the hard work continues. “I keep saying it’s going to be 2035”.
MDMA Treatment
Victims of war or sexual assault are prone to develop anxiety and avoidance behaviors as a result of these tragic experiences. Some of them may be diagnosed with Post-Traumatic Stress Disorder (PTSD), a condition characterized by severe feelings of fear and distress in response to trauma-related details. The increasing prevalence of PTSD is aggravated by the lack of treatment options.
Current trauma-focused psychotherapies, such as exposure and cognitive-behavioral therapy, have important problems of access for certain high-risk populations, as well as high dropout rates. In regard to efficacy, some reviews have found that up to 70% of patients retain their PTSD diagnosis after treatment.
The only two pharmaceuticals with FDA approval also seem to be inefficient for many. One third of all PTSD patients are estimated to be treatment-resistant. This diagnosis is given when several different treatments fail to improve symptoms.
MDMA trials have focused on this specific population because of strategic reasons. It is easier to get permission to test a new drug on patients for whom everything else has failed. Psilocybin trials have taken a similar approach by focusing on treatment-resistant depression or anxiety related to the end of life.
Current clinical research employs a hybrid treatment model that combines the administration of 75 to 125mg of MDMA with therapeutic support provided in preparation and integration sessions. During the drug sessions, therapists monitor the patient and adopt a non-directive approach that allows the person under the effects of MDMA to dive into the experience with minimal interruptions. This model of psychedelic-assisted psychotherapy entails a groundbreaking paradigm in psychiatry that goes beyond mere medications and talk therapy.
A long path
It has taken a while before these modern trials were set up. MDMA is an amphetamine derivative first synthesized by Merck Laboratories in 1912 and later rediscovered by chemist Sasha Shulgin in the 1970s. At the time, psycholytic therapy was being developed with LSD and psychiatrists saw a new potential tool for psychotherapy in MDMA and its empathogenic properties.
Unfortunately, the increasing popularity of “Ecstasy” in recreational contexts and the ensuing anti-drug propaganda soon led to the classification of MDMA as a Schedule 1 substance in 1986, which introduced immense obstacles to scientists investigating its medicinal application.
Ever since, the Multidisciplinary Association for Psychedelic Studies has been working for the approval of MDMA as a therapeutic treatment in mental health and to remove the immense barriers that were thrown up for the potential medication.
Although preliminary investigations by Charles Grob had successfully proved the safety of administration of MDMA to healthy subjects in the 1990s, the first MAPS-sponsored trial for PTSD conducted in Spain by José Carlos Bouso was shut down because of political pressure from the Spanish authorities.
Placebo challenges
So far, six phase-2 clinical trials have been completed, and despite the small samples and the methodological limitations, the results are very promising. The first randomized controlled trials with PTSD patients began to take place in the late 2000s, and resulted in a landmark paper from 2011 by Michael Mithoefer, Mark Wagner, Ann Mithoefer, Lisa Jerome, and Rick Doblin. It concluded that ‘the rate of clinical response was 10/12 (83%) in the active treatment group versus 2/8 (25%) in the placebo group’.
One year later, most of these patients for whom all other treatments had failed still showed a persistent and significant improvement. More importantly, the lack of serious adverse effects pointed at the safety of MDMA in a clinical context and paved the way for more trials.
Skeptics pointed at the methodological weaknesses of this first trial. They criticized the use of lactose as placebo and the difficulties to blind the effects of MDMA to patients and investigators, a common problem in psychedelic therapy trials. An attempt of replication in Switzerland by Peter Oehen which circumvented the blinding problem with an active placebo group (25mg MDMA) showed good results, but were not statistically significant.
Researchers suspected that differences in the work and style of the Swiss therapists might have been behind these suboptimal results, which raised the question of how to standardize the psychotherapeutic part of the treatment. In subsequent trials, MAPS developed an adherence rating system in order to ensure that therapists stick to the standard guidelines of their therapeutic model.
In 2018, Michael Mithoefer published the first dose-response study, which compared the efficacy of three different doses of MDMA: 30mg, 75mg and 125mg. The groups with middle and high doses showed significant remission of PTSD with respectively 86% and 58% of each group’s sample not meeting the diagnostic criteria anymore after treatment, improvements which persisted in the one year follow-up. Shortly after, a similar study by Marcela Ot’alora replicated the results with 76% of patients not meeting the diagnostic criteria for PTSD one year after the treatment.
A Path Towards Regulation
Given these promising results, the FDA accelerated the approval process of MDMA with the Breakthrough Therapy designation in 2017 and allowed the early compassionate use of MDMA-assisted psychotherapy for treatment-resistant patients in 2020.
Two ongoing multi-site phase-3 trials sponsored by MAPS are currently assessing the efficacy of MDMA in around 200 participants from the US, Canada and Israel. Recently, MAPS’ interim analysis of the first phase-3 trial suggested that their results will probably reach statistical significance, and if nothing goes wrong, MDMA could be approved for the treatment of PTSD by mid-2022.
In the meantime, more phase-2 trials are starting to take place in Europe for PTSD and other conditions such as alcoholism. With the first psychedelic substance on the verge of approval, many questions remain in the air:
- What are the psychological and neurobiological mechanisms of action?
- Will psychedelic-assisted psychotherapy become an accessible and affordable, while economically viable treatment option?
- How will the prescription of this unique treatment modality be regulated?
- How will psychedelic therapists be trained?
- How will it be introduced safely and ethically into the mainstream?
All these questions will require years of additional research, which needs to be done by current and future doctors, researchers and policy makers. But the direction and ambition of all this research is clear: to turn the hard facts of well-researched trials into a regulatory model, so that MDMA will be a legal future medication to help many.