In recent years, there has been an increase in interest in the use of psychedelic-assisted therapy (PAT) to help individuals suffering from their addiction. Despite the promising findings from recent clinical trials, many questions remain. How exactly does PAT work to treat addiction? Which different psychedelics are used? What are their potential risks and benefits?
Introduction
Addiction, in its myriad forms, continues to pose a significant challenge to global public health. Recent studies suggest that up to 6% of individuals contend with substance-related issues, with prevalence rates showing an upward trend (Ritchie). Addiction’s cyclical nature, propelled by shifts in brain chemistry, reinforces compulsive behaviors despite adverse outcomes, contributing to a concerning rise in substance-related fatalities. Legal substances like alcohol and tobacco, as per the World Drug Report (2022), account for the primary contributors to morbidity and mortality associated with substance use, while illegal drugs such as psychedelics, amphetamines, and opiates collectively contribute to 5% of the global addiction burden. In the Netherlands, two million individuals are affected by addiction, and in roughly 1,6 million of the cases it involves legal substances such as tobacco and alcohol (LADIS Tussenrapportage Kerncijfers Verslavingszorg, 2016-2021).
The grip of addiction does not only devastate the lives of those afflicted, but it also has a significant impact on families, communities, and society at large. Despite decades of research and numerous interventions, addiction remains a formidable challenge for healthcare professionals worldwide. Indeed, traditional treatment approaches, such as pharmacotherapy and psychotherapy, have demonstrated limited efficacy (Kan; Hayes; Zafar). Research has shown that most individuals often end up relapsing within six months (Hayes), highlighting the need for more innovative solutions. It is within this landscape of unmet medical needs that alternative therapies, such as psychedelic-assisted therapy (PAT), are gaining more and more traction in recent years. It can be considered a novel therapeutic paradigm as it harnesses the psychoactive properties of certain psychedelic drugs to help facilitate the psychotherapeutic process. Unlike conventional addiction treatments that focus solely on symptom management, therapy assisted with psychedelics aims to address the root causes of addiction by inducing transformative experiences that promote introspection, emotional processing, and behavior change, ultimately hoping for long-term recovery.
Defining Addiction
Definition and types of addiction
Addiction is formally defined as the continued use of a harmful substance despite adverse consequences. Core features of addiction include the compulsive pursuit of pleasurable stimuli, fixation on substances or behaviors, and continued engagement despite adverse consequences (Koob, all). Decades of research demonstrate that addiction manifests as a deeply entrenched behavioral pattern influenced by alterations in brain function, environmental factors, and psychological dynamics (Koob, all; Heilig). Repeated substance use induces changes in brain functioning, framing addiction as a neuropsychological disorder.
It’s important to differentiate between two distinct aspects of addiction: controlled substance use and the inability to resist the substance or behavior. These represent separate dimensions that collectively encompass the spectrum of addiction, including drug use, dependence, and abuse.
Controlled substance use refers to instances where an individual may regularly consume a substance, but can manage and regulate their usage without experiencing significant negative consequences. This type of use may not necessarily indicate addiction. On the other hand, the inability to resist substance use or behavior signifies a loss of control, where individuals continue to engage in the behavior despite adverse outcomes. This aspect is characteristic of addiction and encompasses both dependence, where the body becomes reliant on the substance, and abuse, which involves harmful patterns of use. By recognizing these distinctions, we gain a clearer understanding of the multifaceted nature of addiction and can tailor interventions and support accordingly.
In the realm of psychiatry research, addiction is typically classified according to either the DSM-5 or the ICD-11 systems. While DSM-5 is prevalent in research contexts, ICD-11 finds broader application in clinical settings. The DSM-5 conceptualizes addiction along a continuum, whereas the ICD-11 delineates between ‘harmful use’ and ‘dependence.’ Consequently, DSM-5 lacks the detail to distinguish between mild and severe dependence. This variance can significantly impact the interpretation and comparison of addiction studies (Hayes). It’s imperative to note that dependence does not inherently equate to addiction, as dependence primarily relates to tolerance and withdrawal, while addiction encompasses complex behaviors involving drug-seeking and craving (Hayes).
Understanding Addiction
The field of cognitive neuroscience has recently focused on understanding addiction by looking at its genetic, cellular, and molecular mechanisms. Addiction can be defined by an individual’s biology, which helps explain why someone might initially smoke in social settings but eventually become unable to resist despite the high risk of lung cancer. Addiction makes self-regulation difficult, according to Heilig and Koob (2010). Simply put, addiction makes a person have difficulties with self-regulation (Heilig; Koob 2010).
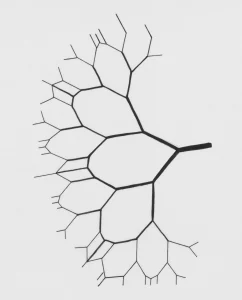
Chronic substance use or harmful behavior significantly impacts neural networks involved in reward processing, inhibitory control, stress response, emotional regulation, and learning/memory, among others, as identified by Koob (2010). One of the most notable findings is that the persistent use of drugs can significantly alter the brain’s structure and function. For example, increases or decreases in the reward system (e.g. ventral striatum) perpetuate cravings, while increases or decreases in the prefrontal region impair self-regulation (Heilig and Koob, 2010).
The disruption of these neural networks has led to several theoretical frameworks that aim to explain how addiction develops over time. Three of the most prominent frameworks include the allostatic hypothesis (Koob, 2005, 2008, 2010), the habit formation theory (Everitt, 2015, 2016), and impaired response inhibition and salience attribution (Goldstein). Despite differing perspectives, all models converge on deficits in reward processing and the hijacking of reward pathways by addictive substances. This leads to prioritizing drug acquisition over non-drug-related pursuits, where the craving for drugs supersedes other goals that are potentially more adaptive for the afflicted individual.
Koob et al.’s (2010) allostatic hypothesis explores addiction through a psychiatric-motivational lens. It suggests that addiction is mediated by cycles of impulsivity and compulsivity delineated in three stages: binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation (craving), depicting dysregulation across three key functional areas (incentive salience/habits, negative emotional states, and executive function, respectively). This process is influenced by three primary neurocircuitry components (basal ganglia, extended amygdala, and prefrontal cortex, respectively).
The hypothesis describes that it starts with excessive drug consumption during the binge/intoxication phase wherein the three stages interact, gradually becoming more intense. Eventually, it leads to a pathological condition that is recognized as addiction. Abstinence of drug intake triggers acute and prolonged withdrawal symptoms during the withdrawal/negative stage, eliciting a secondary motivational urge through negative reinforcement. Negative reinforcement refers to the strengthening of certain behaviors by removing or avoiding negative stimuli or output. Prolonged periods without substance use involve persisting negative emotions and triggered cravings from cues and surroundings, establishing the basis for the preoccupation/anticipation phase (Koob, 2010). The progression from impulsivity to compulsivity underscores addiction’s complex interplay of psychological and neurological factors, marking a shift from reward-seeking to emotion-alleviating and habitual responses.
Current Treatment Approaches and Limitations
Conventional treatment methods typically involving behavioral therapies and medications, have shown only moderate success rates. Studies suggest that a significant number of individuals, particularly those dealing with substance abuse and gambling disorders, tend to relapse within a year of starting treatment (Hayes).
Although pharmaceutical drugs like methadone and naltrexone have been developed to address addiction by reducing withdrawal symptoms and cravings, these interventions may not fully address the underlying causes of addiction, nor do they offer long-lasting solutions for everyone (Peters). For instance, naltrexone, an opioid antagonist, was tested in a double-blind clinical trial on individuals with alcohol dependence and was found to moderately reduce relapse rates. While it does decrease cravings, it does not increase abstinence (Chick). Similar results were observed in opioid dependence, where naltrexone alone did not lead to a decrease in relapses (Gerra).
The chronic relapsing nature of addiction is a significant challenge for clinicians, with limited options available to maintain abstinence. Even for those who have successfully achieved abstinence, the risk of relapse is always apparent, or it seems to never go away. Koob suggests that chronic use eventually leads to increased sensitivity that triggers emotional processes in such a way that encourages drug-seeking behavior. Stress plays a significant role in this relationship and is considered one of the most challenging aspects to address in addiction treatment. Animal studies suggest the role of dopamine and glutamate neurotransmitters in addiction, but craving is difficult to quantify in clinical settings and has not been shown to correlate with relapses (Koob 2008). Nonetheless, further research is required to expand on the knowledge regarding the biological changes in these stages. Understanding the neurocircuitry involved in the progressive stages of addiction lays the groundwork for exploring molecular, genetic, and neuropharmacological adaptations crucial in vulnerability to both the onset and perpetuation of addiction (Koob 2010).
Exploring Psychedelics and Addiction
There has been a growing interest in using psychedelic-assisted therapy to treat individuals suffering from addiction. Classic psychedelics such as LSD, DMT, and psilocybin have been combined with psychological therapy such as cognitive behavioral therapy (CBT) and motivational enhancement therapy (MET). These trials aim to explore the therapeutic potential of psychedelics for various addictions, ranging from alcohol and tobacco to methamphetamine and gambling addiction.
The treatment of addiction leverages the transformative potential of psychedelic drugs when administered in a safe and controlled environment. Early clinical trials and observational studies have shown that psychedelic-assisted therapy sessions can result in notable reductions in substance use, cravings, and relapse rates. Traditional psychedelics may effectively address various addictions, indicating the potential of these substances to target a common underlying mechanism (Yaden).
A pilot study by Bogenschutz (2015) explored the effects of psychedelics on alcohol addiction, particularly with psilocybin. Participants underwent therapy sessions supplemented by psilocybin doses. The results were promising: a significant reduction in drinking days and heavy drinking episodes lasting up to 36 weeks after treatment. Heavy drinking days are defined as when participants consumed more than five drinks for males and more than four drinks for females. The standard drink is settled on 14g alcohol which roughly translates to 130 ml of a glass of red wine or 280 ml of beer. Psilocybin also slashed craving scores by half, offering the potential for long-term recovery. Similar results were suggested in a study of individuals who struggled with tobacco addiction (Johnson, 2014). Psilocybin alongside CBT reported an impressive 80% abstinence rate after six months, far surpassing conventional interventions which contrasts with the typical 35% abstinence rate observed with current therapeutic interventions (Cahill, 2014).
However, these studies are not entirely met with the scientific rigor of randomized controlled studies. For example, open-label studies cannot establish causality. No significant differences were found between moderate and high doses of psilocybin, indicating gaps in understanding its mechanisms in addiction treatment. However, psilocybin-assisted therapy shows lasting impacts beyond the drug’s immediate effects, with participants reporting higher success in quitting smoking when their experiences were highly significant and spiritually meaningful. These findings suggest a potential role of spirituality and the emotion of awe in the effectiveness of psychedelic therapy.
For a deeper exploration, a deep dive into the challenges and knowledge gaps in psychedelic research in addiction treatment and recovery will be taken in the second part of the blog.
In sum, it seems that PAT demonstrates promising outcomes and could offer hope for individuals grappling with addiction. Despite these positive findings, it is important to note that there are still many mysteries in the topic of psychedelics and its potential for treating addiction. As the age-old proverb reverberates within the halls of academia, there is a need for future research so both the efficacy and safety of psychedelics for addiction can be determined.
Meet an Expert in the Field: Dr. Zafar
Dr. Zafar, with his extensive background in neuropsychopharmacology and clinical research, is at the forefront of exploring the therapeutic potential of psychedelics in addiction treatment. His work, conducted within the Centre for Psychedelic Research and Neuropsychopharmacology group, is characterized by a multidisciplinary approach that integrates cutting-edge neuroimaging techniques with clinical interventions.
Dr. Zafar’s involvement in psychedelic therapy for addiction extends beyond research. As a senior scientific officer at Drug Science, he contributes to shaping policy and disseminating evidence-based information on medical psychedelics. Through his consulting and advisory services, he is actively engaged in advancing the field of addiction psychiatry and psychopharmacology.
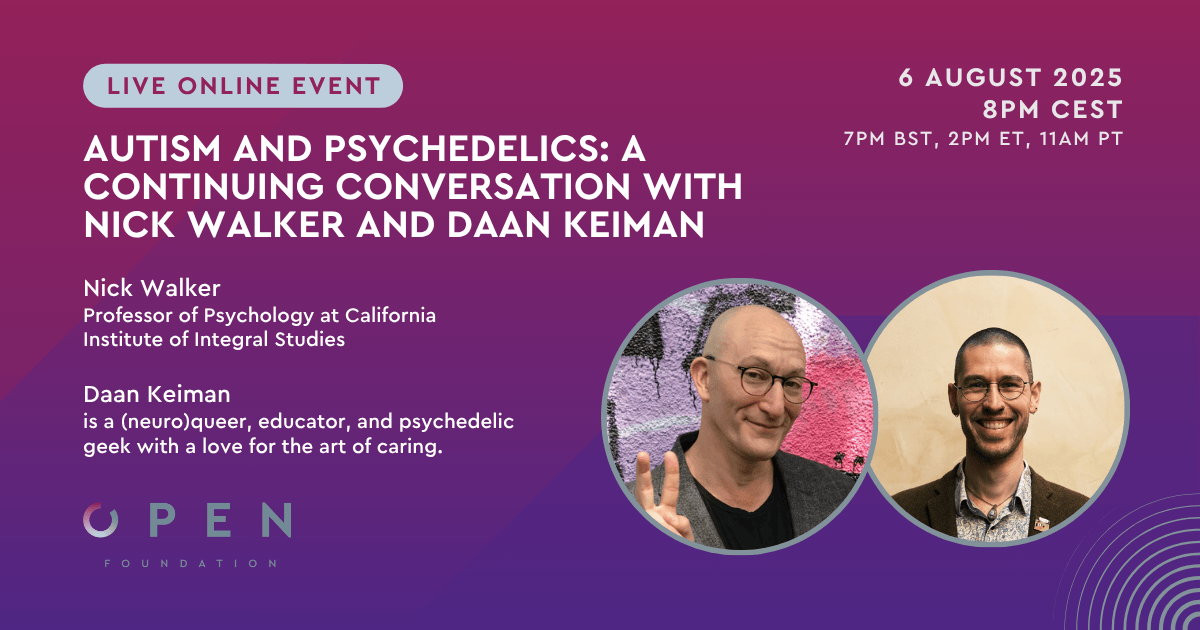
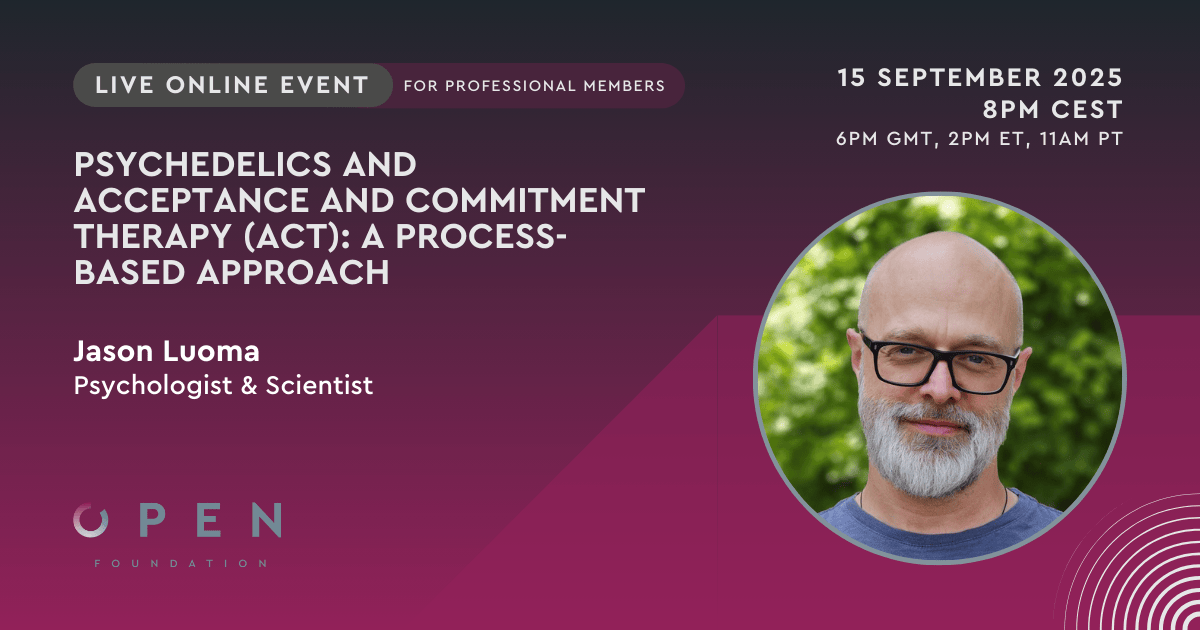
Are you intrigued by Dr. Zafar’s pioneering work in the realm of psychedelic therapy for addiction? Go to part 2 of this blog, where we delve into the insights gleaned from his past online event, shedding light on the dynamic relationship between addiction and psychedelics. Plus, it is possible to gain access to exclusive online events like the one with Dr. Zafar by becoming a member.
By Gwendolyn Drossaert
References
- American Psychiatric Association (1994). Diagnostic and Statistical Manual of Mental Disorders 4th edn. American Psychiatric Press: Washington, DC.
- Bogenschutz, M. P., Forcehimes, A. A., Pommy, J. A., Wilcox, C. E., Barbosa, P. C., & Strassman, R. J. (2015). Psilocybin-assisted treatment for alcohol dependence: a proof-of-concept study. Journal of psychopharmacology, 29(3), 289-299.
- Cahill, K., Stevens, S., & Lancaster, T. (2014). Pharmacological treatments for smoking cessation. Jama, 311(2), 193-194.
- Chick, J., Anton, R., Checinski, K., Croop, R., Drummond, D. C., Farmer, R., … & Ritson, B. (2000). A multicentre, randomized, double-blind, placebo-controlled trial of naltrexone in the treatment of alcohol dependence or abuse. Alcohol and alcoholism, 35(6), 587-593.
- Everitt, B. J., & Robbins, T. W. (2016). Drug addiction: updating actions to habits to compulsions ten years on. Annual review of psychology, 67, 23-50.
- Everitt, B. J., & Robbins, T. W. (2005). Neural systems of reinforcement for drug addiction: from actions to habits to compulsion. Nature neuroscience, 8(11), 1481-1489.
- Gerra, G., Fantoma, A., & Zaimovic, A. (2006). Naltrexone and buprenorphine combination in the treatment of opioid dependence. Journal of psychopharmacology, 20(6), 806-814.
- Goldstein, R. Z., & Volkow, N. D. (2011). Dysfunction of the prefrontal cortex in addiction: neuroimaging findings and clinical implications. Nature reviews neuroscience, 12(11), 652-669.
- Griffiths, R. R., Richards, W. A., Johnson, M. W., McCann, U. D., & Jesse, R. (2008). Mystical-type experiences occasioned by psilocybin mediate the attribution of personal meaning and spiritual significance 14 months later. Journal of psychopharmacology, 22(6), 621-632.
- Hayes, A., Herlinger, K., Paterson, L., & Lingford-Hughes, A. (2020). The neurobiology of substance use and addiction: evidence from neuroimaging and relevance to treatment. BJPsych Advances, 26(6), 367-378.
- Heilig, M., MacKillop, J., Martinez, D., Rehm, J., Leggio, L., & Vanderschuren, L. J. (2021). Addiction as a brain disease revised: why it still matters, and the need for consilience. Neuropsychopharmacology, 46(10), 1715-1723.
- Johnson, M. W., Garcia-Romeu, A., Cosimano, M. P., & Griffiths, R. R. (2014). Pilot study of the 5-HT2AR agonist psilocybin in the treatment of tobacco addiction. Journal of psychopharmacology, 28(11), 983-992.
- Johnson, M. W., Garcia-Romeu, A., & Griffiths, R. R. (2017). Long-term follow-up of psilocybin-facilitated smoking cessation. The American journal of drug and alcohol abuse, 43(1), 55-60.
- Kang, M., Mackay, L., Christie, D., Callon, C., & Argento, E. (2022). Can psychedelic-assisted psychotherapy play a role in enhancing motivation to change in addiction treatment settings?. Journal of Psychedelic Studies.
- Koob, G. F., & Le Moal, M. (2008). Addiction and the brain antireward system. Annu. Rev. Psychol., 59, 29-53.
- Koob, G. F., & Le Moal, M. (2005). Plasticity of reward neurocircuitry and the’dark side’of drug addiction. Nature neuroscience, 8(11), 1442-1444.
- Koob, G. F., & Volkow, N. D. (2010). Neurocircuitry of addiction. Neuropsychopharmacology, 35(1), 217-238.
- LADIS Tussenrapportage Kerncijfers Verslavingszorg 2016-2021, IVZ (2023) see link: https://cdn.bluenotion.nl/209c705755afb5baca6501d22c0ddc6e05c586540b8868fe813b7a1b3cb76695.pdf
- Peters, J., & Olson, D. E. (2021). Engineering safer psychedelics for treating addiction. Neuroscience Insights, 16, 26331055211033847.
- Ritchie, H., Arriagada, P., & Roser, M. (2022). Opioids, cocaine, cannabis and other illicit drugs. Our World in Data.
- World Drug Report 2022: https://www.unodc.org/unodc/data-and-analysis/world-drug-report-2022.html
- Yaden, D. B., Berghella, A. P., Regier, P. S., Garcia-Romeu, A., Johnson, M. W., & Hendricks, P. S. (2021). Classic psychedelics in the treatment of substance use disorder: potential synergies with twelve-step programs. International Journal of Drug Policy, 98, 103380.
- Zafar, R., Siegel, M., Harding, R., Barba, T., Agnorelli, C., Suseelan, S., … & Erritzoe, D. (2023). Psychedelic therapy in the treatment of addiction: the past, present and future. Frontiers in Psychiatry, 14, 1183740.