Abstract
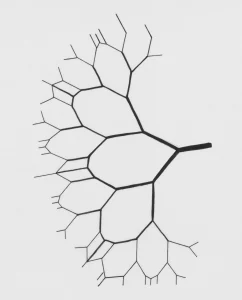
The indole alkaloid ibogaine, present in the root bark of the West African rain forest shrub Tabernanthe iboga, has been adopted in the West as a treatment for drug dependence. Treatment of patients requires large doses of the alkaloid to cause hallucinations, an alleged integral part of the patient’s treatment regime. However, case reports and case series continue to describe evidences of ataxia, gastrointestinal distress, ventricular arrhythmias and sudden and unexplained deaths of patients undergoing treatment for drug dependence. High doses of ibogaine act on several classes of neurological receptors and transporters to achieve pharmacological responses associated with drug aversion; limited toxicology research suggests that intraperitoneal doses used to successfully treat rodents, for example, have also been shown to cause neuronal injury (purkinje cells) in the rat cerebellum. Limited research suggests lethality in rodents by the oral route can be achieved at approximately 263mg/kg body weight. To consider an appropriate and safe initial dose for humans, necessary safety factors need to be applied to the animal data; these would include factors such as intra- and inter-species variability and for susceptible people in a population (such as drug users). A calculated initial dose to treat patients could be approximated at 0.87mg/kg body weight, substantially lower than those presently being administered to treat drug users. Morbidities and mortalities will continue to occur unless practitioners reconsider doses being administered to their susceptible patients.
Schep, L. J., Slaughter, R. J., Galea, S., & Newcombe, D. (2016). Ibogaine for treating drug dependence. What is a safe dose?. Drug and alcohol dependence, 166, 1-5. 10.1016/j.drugalcdep.2016.07.005
Link to full text
Schep, L. J., Slaughter, R. J., Galea, S., & Newcombe, D. (2016). Ibogaine for treating drug dependence. What is a safe dose?. Drug and alcohol dependence, 166, 1-5. 10.1016/j.drugalcdep.2016.07.005
Link to full text